Scarring Alopecia
Scarring Alopecia can have devastating affects on patients. Furthermore the hair is destroyed as a result the skin may show some horrendous disfigurements therefore you are advised to seek professional advice in the first instance. You will see the affects in some of the images below. The symptoms vary because skin reacts differently from person to person. They include minor or major pruritus (itching), Erythema (red skin). Swelling, burning, pain, over production of sebum, heat etc etc. The list goes on therefore if you are showing symptoms such as the above then please seek professional advice.
Most patients will go and see their GP as it seems like the normal thing to do. While some have specialists skills in skin most GPs are not specialists.. Sadly, through experience some GPs are reluctant to send you to a specialist under the NHS. Unless you have a firm diagnosis you don’t know what you are dealing with. Therefore you don’t know if you have the right treatment hence the importance of seeking the right advice. Many scarring alopecia can destroy hair quickly. Most noteworthy you WILL NOT be able to grow the hair back!.
Finally, at the Holborn Clinic we have specialists that advice and treat such ailments. Therefore have a read through this page and see if this sounds like what you have. Alternatively, you can give us a ring and have a chat.
Consultation Scarring Alopecia
Booking a consultation at the Holborn Clinic couldn’t be easier. Just give us a ring or fill I the short contact form and we will get back to you. We will speak to you first to gauge the severity. We ask that you are as open as you can be with us to allow us to give the best advice. In most cases the best advice is to attend the Holborn Clinic and have a consultation with a registered Trichologist (The Trichological Society TTS). We specialist is diseases of the scalp. Remember, once the hair has gone it will not return. Spending a little time and effort could just save your hair and prevent the scarring alopecia from getting worse. Thank you for taking the time to read our site.
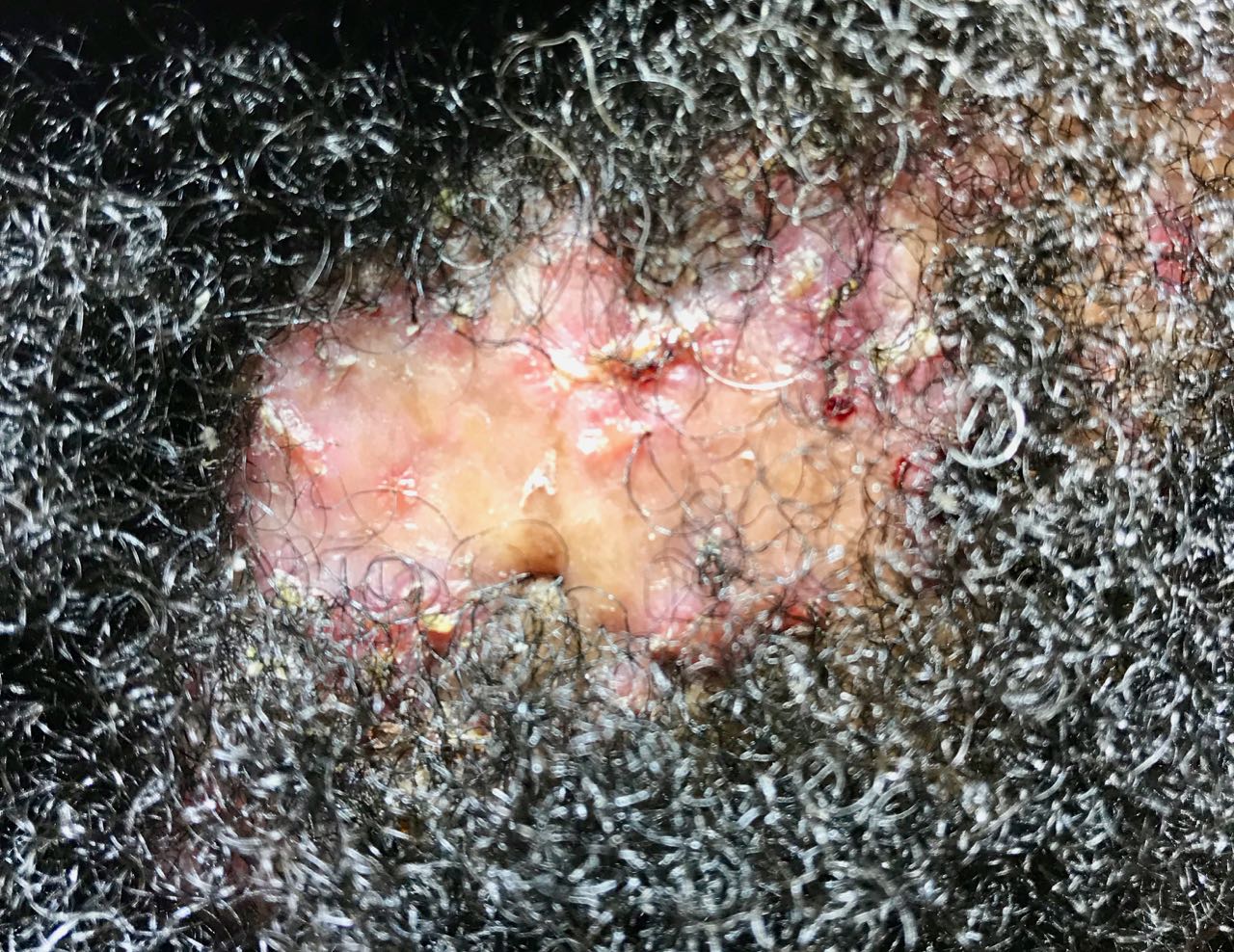
Folliculitis Decalvans
A scarring alopecia that is characterised by the presence of pustules around the hair follicle resulting in permanent loss of hair accompanied by follicle destruction and scarring. The scarring alopecia affects both men and women. The onset can occur any time after adolescence. Aetiology is uncertain, but staphylococcus aureus has been implicated. Folliculitis Devalvans destroys the hair over time leaving unsightly scar tissue. Symptoms include pruritus, burning, erythema, pain, lack of sleep and hair loss.
Treatments tend to be that of antibiotics that must continue throughout the duration of the conditions which means you will be taking antibiotics potentially for years. We have methods that may assist avoiding the use of allopathic medicines. You must seek professional advice to deal with this ailment before it destroys your hair for good.

Acne Necrotica
Acne in many cases will cause scarring alopecia if not dealt with correctly. Afro Scalps are particularly susceptible and the scars may lead to keloids because of its destructive nature. Spots will appear that become painful and inflamed are the primary symptoms. A common ailment which can be controlled. Curing Acne may not be possible. The use of steroid lotions and creams or antibiotics tend to be the obvious treatment methods. We at the Holborn Clinic have treatment that offer support to the immune system and assists in controlling the condition in most cases.
Impetigo Scarring Alopecia
A skin infection caused primarily by the presence of Group A Beta-hemolytic Streptococci (GABS) aka Streptococcus Pyogenes. Staphylococcus Aureus can also be isolated from impetigo lesions. Impetigo presents as small blisters which rapidly coalesce and rupture. The thin yellow exudate dries forming a crust. The scalp, legs, arms, face and trunk may be affected. Incubation period-up to 10 days. Hair losses and scarring may occur.
Causes: direct skin-to-skin contact with a carrier or someone suffering streptococcal pharyngitis.
Treatment: aural / topical antibiotic.
Hyperkeratosis Cystica Follicularis – A rare scarring alopecia which presents as greatly dilated follicles with horny plugs. Has been attributed to a folliculitis with keratotic micro cysts.
Herpes Zoster (Shingles) – Scalp Shingles presents as a localised rash with blistering (cause: Varicella the chickenpox virus). The blisters burst and crust over usually within a week often leaving pale scars. This condition may be painful. Scarring alopecia may follow.
Treatment: is to relieve pain (analgesics), or a non-steroidal anti-inflammatory medicine. Calamine lotion may help.
Pseudo-pelade (Brocq)
Early stages shows similarities to alopecia areata presenting as one or more small bald patches which are smooth and atrophic. Many more such patches may appear. Affected areas include the scalp, in particular the vertices and parietal regions. Also known as footsteps in the snow.

Frontal Fibrosing Alopecia
Frontal Fibrosing Alopecia is a scarring alopecia that affects women post menopause. Resulting in the loss of the frontal hair line often mistaken for female pattern baldness. The hair follicles become inflamed and very itchy. They skin is red and will show follicular plugging. The hair follicles are gradually destroyed over time leaving a shiny forehead void of all hair. The condition will eventually stop but the amount of hair it destroys varies.
If you see your frontal hair line receding as a female then seek professional advice as soon as possible. I have seen several cases over the years where patients have been wrongly diagnosed resulting in permanent hair loss. Some suggest this condition is in fact Lichen Planus.
At the Holborn Clinic we have methods that can assist in the slowing and stopping of frontal Fibrosing Alopecia. Please feel free to give us a call to find out more.

Lichen Planus (Planopilaris)
Lichen Planopilaris (scalp lichen planus) presents as follicular and perifollicular violaceous, scaly, pruritic scalp papules which may coalesce into plaques. Hairloss and cicatrix may follow. The disease tends to affect women and causes cicatrical alopecia with inflammation around affected hair follicles. In middle-aged patients distinct bald patches are exhibited. Pseudopelade may be the diagnosis. The skin may present a purple appearance and often concave. A biopsy is often needed to aid diagnosis. Treatment: Oral / topical steroids may be helpful.
Lupus Erythematosus (discoid & systemic)
A chronic inflammatory condition caused by an autoimmune disease (tissue attacked by its own immune system). Antibodies fight infectious agents. Lupus sufferers produce abnormal antibodies which target own-body tissue rather than foreign infectious agents. This condition can cause many and varied diseases. It presents itself as:
i) Discoid Lupus Erythematosus – affecting the skin.
ii) Systemic Lupus Erythematosus – internal organs are involved
First of all, Lupus is frequently seen in Mongoloid and Negroid women. Furthermore the disease can affect all age groups but more frequently commences in those aged 20 to 45 years. Its precise cause remain uncertain but genetics, viruses, exposure to ultraviolet light, and various drugs are suspected. Consequently, discoid lupus is usually painless and non-pruritic but often results in scarring alopecia which may become extensive.
Tufted Folliculitis
Another scarring alopecia known as Tufted Folliculitis. A rare scalp folliculitis that presents as an uncomfortable erythematous skin with adherent crust and follicular hyperkeratosis. Multiple hairshafts (5-12) may emerge from single dilated follicles. these hairshafts may depigment. Lesions are often symmetrical. most noteworthy, Response to topical (intralesional) or systemic treatments is uncertain. In contrast, reviewing this under a microscope will present the illusion of palm trees.
Traction Scarring Alopecia
Scarring Alopecia which is often permanent. Tends to affect girls and women (afroid and caucasoid) because they tend to have long hair. Tends to affect the anterior margins, auriculars and occipital hair line because this is where the most strain is placed. This hair loss will lead to a degree of permanents as a result of scalp trauma produced by plaits, cornrows, long hair dressed and maintained firmly in chignons, ponytails, pleats etc. Similar damage may occur elsewhere on the scalp associated with hair extensions, tracks and the tight application of styling rollers.
Finally, If you would like further information or would like to speak with a trichologist please contact give us a call on the number above. Likewise you can contact us by completing the form above. We hope you have found this page informative.
Registered Scarring Alopecia Trichologists – The Trichological Society TTS